An Herbalist’s Advice on COVID-19, Influenza, and Other Flu-Like Viruses
Rachel Fee, Trauma-Informed Herbalist and Earthaven resident and member, weighs in on which herbs may be truly helpful for prevention and treatment with COVID-19, which may be dangerous or unhelpful, and why.
Here is a timely perspective from one of our resident Earthaven herbalists on supporting our immune systems and treating lung-affecting diseases. Originally shared within the Earthaven community, SOIL is glad to have permission to share this information with our wider web of connections in hopes it will be helpful to those who plan to use herbs as part of their personal and family care protocols during the crisis.
Rachel Fee is a Trauma-Informed Herbalist whose professional interests include infectious disease and bioregional herbal practices. In the wake of a sudden deluge of information and advice related to the prevention and treatment of COVID-19, Rachel speaks from her clinical experience to address some of the misguided advice in circulation. She suggests safe and effective protocols suited to energetic presentation of this particular virus as we understand it so far.

On ‘Antivirals’, and The Importance of Energetics
In light of the pandemic, herbs categorized as antivirals have become a focus of public attention. Rachel explains, however, that the term may be misleading, contributing to misunderstanding about the difference between what is effective for deactivating viruses in direct contact vs ones they have entered our bodies:
“If you want herbs to kill a virus, you’ll be disappointed. Using words like antibiotic and antiviral lead to a lot of misunderstanding about how herbs work in our bodies. Yes, in petri dishes and with direct contact, there are herbs that inhibit virus replication or kill bacteria (e.g. essential oils do make great hand and surface sanitizers).
Many non-clinical herbalists will write books about that, not discerning between what is proven true in a lab and what is proven true in our bodies.”
Rachel warns against a this-for-that approach to matching herbs to symptoms, explaining why it is crucial to account for the energetic qualities of herbs, bodies, and disease patterns:
“As a practitioner, I love tradition and science, but I love energetics more. The nuance that comes with knowing the qualities of an herb (warming, drying, moistening, cold, etc.) and being able to match those with the energetics of symptom presentation in a certain individual are my jam.
Treat enough folks, and you quickly learn what is mythological and what works. Matching herbs to an illness usually doesn’t work.
Echinacea for the immune system, St John’s Wort for depression, etc., while containing a kernel of partial truth, has no nuance whatsoever.”
She draws a helpful analogy between how a skilled permaculturist would approach a piece of land they wish to garden, and how we benefit in using a similar holistic thinking when assessing the terrain of the body to make specific and effective treatment choices:
“Would you walk onto a piece of land and make plans for living on it and farming it without taking into account the land itself? Would you grow the same crop year after year in the same place and never tend to the soil?
As we know, soils from different places, even in the same field, need different amendments. Bodies are similar in this regard. We have to “permacultureize” how we think about our bodies and our health. We have to take the terrain into account.
Since the introduction of germ theory, and the miracle drug of antibiotics, the societal narrative has increasingly shifted to ignoring the state of the body and focusing on killing the invader. It’s true, once bacteria or viral infection takes hold, it is hard to treat.
However, strep, staph, and all manner of things live in our bodies all the time, taking hold when the terrain changes. Bacteria LOVE a damp spongy tissue to thrive in, and that’s where our herbal medicines excel.”
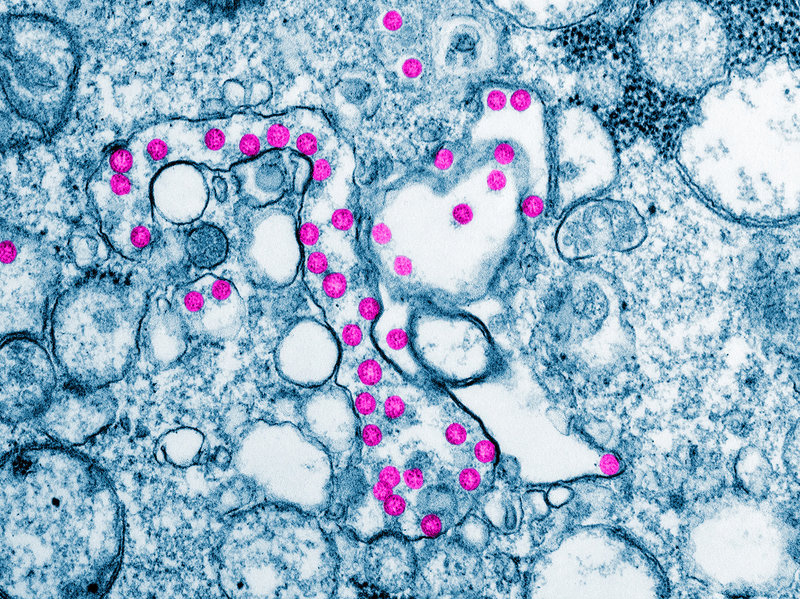
Energetic Presentation of COVID-19 and Advice on Fevers
So what is the ‘terrain’ we are working with when preventing or treating coronavirus infections? While each individual’s underlying body constitution and health history will determine which herbs are appropriate in their case, there are also broad patterns of energetic presentation to COVID-19 symptoms which should guide choices in remedies:
“Initial reports from China from herbalists like Thomas Avery Garran, a Traditional Chinese Medicine practitioner living in Beijing, indicated that it is a cold, damp condition in the lungs. However, most cases observed by herbalists in the U.S. have seen a dry lung presentation with an unproductive cough.”
Fever is one of the most common symptoms of the infection. Rachel addresses the healing value of allowing fevers to work without interference, and why she advises people not to reach for NSAIDS or herbs in order to suppress a normal fever:
“Most will present with a fever. Let that fever have its way! It’s the body’s first-line-of-defense immune response. Breaking it will make the inflammatory stage worse and increase the likelihood of secondary infection like pneumonia.
Sudden onset and sustained high temps are a different story and more serious. If someone becomes excessively lethargic and minimally responsive, that’s the time to lower a fever and be concerned.
It’s uncomfortable, but a fever is our body’s most effective way of dealing with bacterial and viral invaders. Stick to water, infusions, and broths. Don’t saddle the body with the additional burden of digestion. Stay in bed and well hydrated. Don’t obsess over the number on the thermometer.
Even though there’s a fever, something “hot”, present, the underlying cause is the dry, constricted condition in the lungs. That’s what we really want to treat. NSAIDS suppress immunity and increase the likelihood of secondary infections and severe complications.”
Cytokine Storms, And Herbs NOT to Use During Infection
Much attention has been placed on the concept of ‘boosting’ our immune systems, along with recommendations circulating to lean on some of our most trusted standby herbs such as echinacea and medicinal mushrooms for infections.
Rachel explains why some of these otherwise helpful allies may be unhelpful, and even dangerous choices, when working specifically with COVID-19 and other viruses which can lead to pneumonia.
“Most of what we think of as immune system boosters up-regulate the production of various cytokines in the body. As you may have heard, “cytokine storm” is what is responsible for many deaths from Covid-19, H1N1, etc. Generally, cytokine surges are rare occurrences and do not happen in healthy children and adults and we should not be overly concerned about this phenomenon.
Echinacea, reishi and other mushrooms, astragalus, elderberry, and colloidal silver all up-regulate cytokines that are indicated in these new viruses. There are reports of cytokine storms being induced by elderberry and colloidal silver specifically during the swine flu epidemic.
Unfortunately, we don’t have enough context to know what the individual’s foundational health was like and if they had any pre-existing conditions or underlying factors for a cytokine storm or if they were healthy low risk individuals and the remedies really are responsible.
That doesn’t mean not to take them now, but to discontinue use if you become symptomatic. This is wise with any virus like the flu or common cold.
If you persist in taking these herbs that increase killer cells, you are basically ramping up the body’s inflammatory response and making your symptoms worse; more and longer lasting mucous production, possible secondary infections, etc.
It’s very likely that one would already have sought out medical attention for severe symptoms before the conditions for a cytokine storm coalesce. A few doses of elderberry won’t do it. However, those with autoimmune disorders and immunosuppression should be cautious. ”
Colloidal Silver and Respiratory Disease
She adds a warning from her experience with colloidal silver:
“Since I mentioned colloidal silver, I do not trust or use this as a remedy. The science is questionable at best, and all of it that is reputable is done on topical, not internal, use. It does seem to have some merit topically as a wound wash. The questions are many, and in my experience, the benefits few.”

Herbal Recommendations for Prevention and Treatment
She addresses the plants she relies on to nourish her own family for prevention, and the importance of nourishing the nervous system, too:
“Personally, I am currently using elderberry and elderflower for me and my family, along with tulsi and ginger. Um, it’s delicious, too. Tulsi has all the qualities people want to label as antibacterial and antiviral, as well as down regulating the inflammatory process, tonifying the endocrine and CNS (central nervous system) so that we can better weather the stress of dealing with this crisis.
At the time any of us has fever or serious respiratory symptoms, I’ll discontinue the elderberry.”

Other excellent preventatives are ginger and turmeric. Both down regulate inflammation while having the proper energetics for this illness (warming and relaxing)… Actually, chai is really perfect for this situation. It’s supportive of immune function, and all of those delicious aromatic spices are, you guessed it, warming and relaxing to mucous membranes.
This is a dry presentation, so add violet leaf or marshmallow to your chai for some healthy moistening demulcent action. Overly dry lungs tend to overproduce mucus which gives viruses and bacteria a happy home. So we are looking for a Goldilocks situation: not too dry, not too wet. Chai, as a preventative measure, also crosses into the treatment category.”

Once an infected individual has respiratory symptoms, some of the most helpful remedies happen to be common and easy-to-find culinary herbs many already have at home:
“Those warming aromatic spices: ginger, cinnamon, clove, nutmeg, cardamom, black pepper, anise, turmeric, etc., along with others like thyme, rosemary, and oregano are perfect for treating the symptomatic, or inflammatory, stage of a virus.
Cayenne, horseradish, and garlic are also indicated here when I normally wouldn’t advise them. They are HOT and extremely DRY. In a lot of conditions, this is too much heat and irritation to the mucosa, but appropriate when the proper moistening herbs are used for balance.
Raw garlic infused into half ACV half honey is the most balanced delivery system in my experience.”

Some external and topical remedies Rachel recommends:
“Mustard plasters and onion poultices are specific for constricted lung conditions. Use hot steams with eucalyptus, thyme, tea tree, rosemary essential oil and salt to thin mucus. Lungs are cooler than body temperature, so this is helpful for prevention and treatment as it makes the tissues less inhabitable for heat sensitive viruses.
Take baths in hemlock, or prepare a hemlock or pine oil to rub on the chest. All are warming, stimulating, and relaxing.”
Other plants which are supportive in managing mucus/wet cough which this condition may evolve into as it unfolds in individual bodies:
“Elecampane, mullein, thyme, and cherry bark will help expel mucus. I especially love a wild cherry bark syrup with anise, cinnamon, and ginger for this. So effective.
Spicebush berries, birch, Japanese knotweed, willow, chamomile and plantain should probably be mentioned here. They are all going to help manage the respiratory inflammation, along with elder, yarrow and garlic being helpful in responding to the virus itself.”

More Info
Local Remedies Grow Resilience
Much as the COVID-19 crisis makes visible the increasing dangers of globalism and illuminates the crucial importance of transitioning towards local and bioregional economies, many of the most effective protocols we can use to treat ourselves are in fact bio-regionally abundant plants, and common culinary herbs.
Rachel steers us away from industrial paradigms of healing towards more sustainable and effective strategies:
“None of these suggestions are super sexy or terribly exotic, but they work. What can I say? I’m proud to be a boring herbalist. Which brings me to heroic measures: We don’t need fancy, hard to find, exotic herbs.
Herbs don’t have to be exciting, toxic, or a hammer over the head to be effective. Gentle doesn’t mean impotent. Let’s decolonize and de-industrialize our herbal practices.”
As advised, let’s remain aware of our underlying constitutions when applying these suggestions – or any other herbal advice – to our own situation!
When in question, please reach out to a trusted and experienced professional herbalist for consultation. Rachel is available for consultation on request, and can be reached at [email protected].
An Update from SOIL
On behalf of the entire SOIL team, we are wishing all in our extended community and their loved ones continued resilience, wellbeing, and togetherness at this time. We look forward to continuing in the work of sharing whole-life skills for community resilience which are so deeply needed at this moment and for the health of our shared future.
Like so many schools and places of business, we are pausing in-person gatherings in the near future. Our 2020 programs have been rescheduled to 2021, beginning in May.
Please stay in touch with us via our monthly newsletter to be in the loop about changes to our program schedule, updates as programs resume, important information like in this article, and to keep up with other happenings at SOIL.
**This article is not intended to be a substitute for professional medical advice. Always seek the counsel of your physician or other qualified medical provider with questions. Please refer to the WHO (World Health Organization) emergencies page and the CDC (Centers for Disease Control) for official updates and recommendations about the COVID-19 outbreak or other respiratory diseases.